Struggling with stubborn patches, constant itching, or recurring flare-ups? If you’re looking for psoriasis treatment in Jaipur, you’re not alone. Psoriasis is a long-term, immune-related skin condition that doesn’t just affect the skin—it can impact confidence, sleep, work, and overall quality of life.
At Dermacian – Skin & Hair Clinic, Jaipur, our skin specialists for psoriasis combine advanced medical treatments with personalised care to help patients gain lasting relief. From modern phototherapy and topical solutions to systemic medicines and biologics, we offer evidence-based options tailored to your needs.
This blog will walk you through the causes, symptoms, and challenges of psoriasis, highlight the professional treatments available at Dermacian, and share dermatologist-approved home care tips to help you manage flare-ups more effectively.
Psoriasis at a Glance: Causes, Symptoms & Everyday Problems
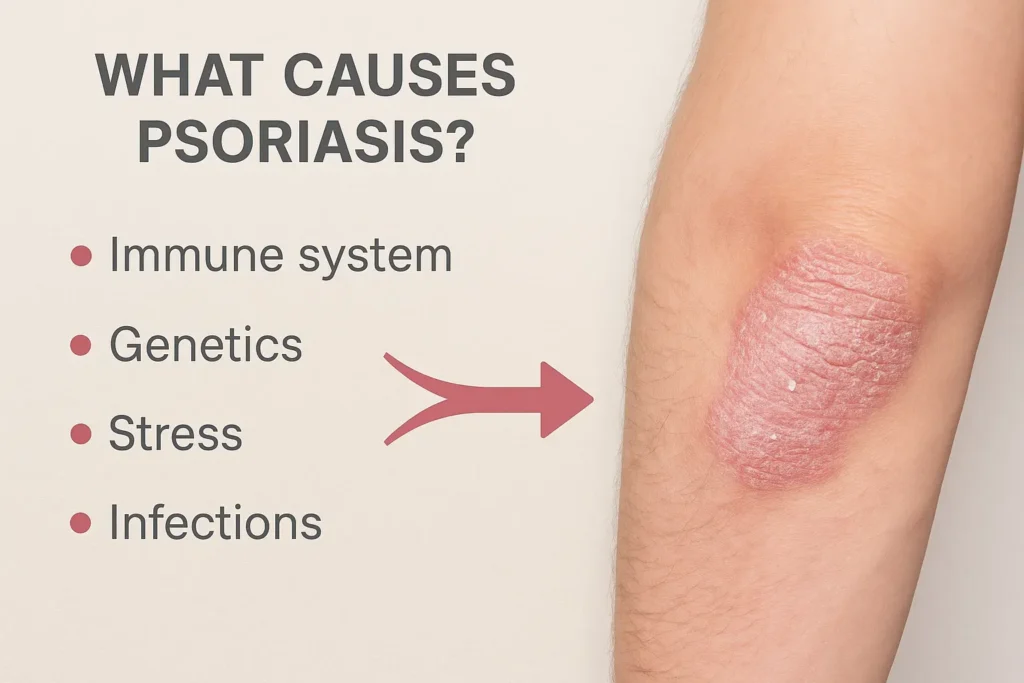
What causes psoriasis?
Psoriasis happens when the immune system speeds up skin cell turnover, causing red, inflamed, scaly plaques. While the exact cause is complex, these factors often play a role:
- Genetics: Family history increases risk.
- Immune triggers: Infections (especially throat infections), injuries to skin (Koebner phenomenon), and chronic inflammation.
- Lifestyle & environment: Stress, cold/dry weather, smoking, alcohol.
- Certain medications: Some blood-pressure medicines (beta-blockers), lithium, and others can aggravate psoriasis.
- Metabolic health: Obesity and insulin resistance can worsen severity.
Read More: Top Fungal Infection Doctor in Jaipur: Diagnosis, Treatment & Prevention
How do symptoms look and feel?
Common signs vary by type and body site:
- Plaque psoriasis: Raised, red patches with silvery scales on elbows, knees, back, and scalp; often itchy or sore.
- Scalp psoriasis: Flaky, adherent scales with redness; can resemble stubborn dandruff.
- Guttate psoriasis: Small drop-like spots, often after a throat infection (frequent in younger patients).
- Palmoplantar psoriasis: Thick scaling on palms and soles; may crack and hurt.
- Nail psoriasis: Pitting, discolouration, thickening or lifting of the nail.
- Psoriatic arthritis: Joint pain/stiffness—especially morning stiffness—warrants early evaluation.
Why does psoriasis feel so hard to manage?
- Relapsing pattern: Good phases and flare-ups can be unpredictable.
- Itch, burn, and pain: Discomfort affects sleep and mood.
- Visible impact: Patches on face, scalp, or hands can dent self-esteem.
- Treatment myths: “Steroids are the only option” or “It’s just dandruff” delay proper care.
- Self-medication risks: Unsupervised steroid use can thin skin and worsen rebound flares.
Professional Psoriasis Treatments at Dermacian (Jaipur)
At Dermacian, our dermatologists create personalised, step-wise plans based on disease type, severity, body sites, age, lifestyle, and co-existing conditions. We use evidence-based therapies with close monitoring for safety and results.
1) Precise assessment & baseline planning
- Dermatologist examination to identify type (plaque, scalp, nail, guttate, palmoplantar).
- Severity scoring & photo-tracking to monitor progress objectively.
- Trigger mapping (stress, infection, weather, products, medicines).
- Co-morbidities screening (obesity, metabolic syndrome, arthritis).
2) Medical treatments we commonly use
Topical therapy (first-line for many)
- Corticosteroids (correct potency, limited duration, safe taper).
- Vitamin D analogues (calcipotriol) and combination gels/ointments for better control.
- Keratolytics (salicylic acid) to lift scales and enhance penetration.
- Calcineurin inhibitors (for delicate areas like face or skin folds).
Phototherapy (clinic-based)
- Narrowband UVB (NB-UVB): Gold-standard light therapy for widespread disease; non-invasive and suitable for many age groups.
- Targeted 308-nm excimer device: Focused light for stubborn plaques, scalp margins, elbows/knees, and limited-area disease.
Systemic medicines (for moderate–severe or resistant cases)
- Methotrexate or cyclosporine (short-term induction) with lab monitoring.
- Apremilast (oral small-molecule) for patients preferring needle-free options.
- Retinoids (acitretin) for thick plaques and palmoplantar disease.
Biologics (advanced targeted therapy)
- For extensive or disabling psoriasis and psoriatic arthritis, our dermatologists consider biologics (e.g., anti-TNF, anti-IL-17, anti-IL-23 agents) after evaluating indications, screening tests, and safety. These can deliver rapid clearance with maintenance schedules tailored to you.
Special care programs
- Scalp psoriasis protocols: Medicated shampoos, steroid-vitamin D lotions, keratolytic oils, and clinic-delivered targeted light.
- Nail psoriasis management: Topicals, intralesional therapy (where indicated), and systemic options for significant nail disease.
- Arthritis co-management: Dermatology–rheumatology referral pathway if joint pain or swelling is present.
3) Safety first: monitoring & follow-ups
- Structured follow-up to track response, side effects, and step-down planning.
- Lab monitoring when on systemic therapy.
- Relapse-prevention education to extend clear periods.
4) How fast will I see results? What about cost?
- Topicals: Early improvements often in 2–4 weeks with correct use.
- Phototherapy: Noticeable clearing often from week 3–6 with scheduled sessions.
- Systemics/biologics: Some agents show response by weeks 2–4; full benefit typically over 8–12+ weeks.
- Costs: Depend on severity, chosen therapy (e.g., light-therapy packages vs. oral medicines vs. biologics) and follow-up frequency. You’ll receive a transparent plan and estimate during consultation.
Quick comparison of options
| Treatment | Best For | Clinic or Home | Typical Onset* | Notes |
| Topical steroids + Vitamin D | Mild–moderate, limited areas | Home | 2–4 weeks | Correct potency & tapering prevent side effects |
| NB-UVB phototherapy | Moderate, widespread, pregnancy-friendly | Clinic | 3–6 weeks | Non-invasive; requires scheduled sessions |
| Excimer (targeted light) | Stubborn plaques, scalp margins | Clinic | 2–5 weeks | Focused on small areas; fewer sessions per spot |
| Methotrexate/Apremilast | Moderate–severe, palmoplantar, nail | Home (with check-ups) | 2–8 weeks | Periodic labs/monitoring as advised |
| Biologics | Severe psoriasis / arthritis | Clinic-guided | 2–12 weeks | Highly effective; screening & schedule essential |
*Onset varies by individual and adherence.
Read More: Vitiligo Treatment in Jaipur: Causes, Options & Expert Care at Dermacian
Home Remedies & Lifestyle Tips for Psoriasis (Dermatologist-Approved)
Psoriasis may be a long-term condition, but the way you care for your skin daily has a direct impact on flare-ups, comfort, and confidence. These lifestyle adjustments don’t replace medical treatment, but they work alongside it to enhance results, prevent relapses, and make living with psoriasis easier.
Dermatologist-Approved Lifestyle Tips
1. Keep skin well-hydrated
Apply a thick, fragrance-free moisturiser immediately after bathing and reapply on dry or itchy patches throughout the day. A strong skin barrier means less dryness, cracking, and irritation.
2. Practice gentle bathing
Choose lukewarm water, limit shower time, and use mild cleansers instead of harsh soaps. Avoid scrubbing, as it can worsen irritation and trigger new patches.
3. Care for your scalp
If you have scalp psoriasis, use prescribed medicated shampoos. Apply emollient oils before wash days to soften scales and make cleansing more effective.
4. Take in safe sunlight
A few minutes of early-morning sunlight may reduce symptoms. Avoid peak sun hours and never allow skin to burn, as sun damage can worsen psoriasis.
5. Manage stress effectively
Stress is a common trigger. Incorporate relaxation techniques such as meditation, yoga, breathing exercises, or calming hobbies to reduce flare frequency.
6. Focus on diet and movement
An anti-inflammatory lifestyle supports skin health. Eat more fresh fruits, vegetables, whole grains, lean proteins, and omega-3-rich foods. Maintaining a healthy weight and staying active also reduces the severity of psoriasis.
7. Identify personal triggers
Keep a simple diary of flare-ups and note possible causes such as infections, weather changes, or new medications. Sharing this with your dermatologist helps fine-tune treatment.
8. Avoid self-medicating with steroids
Potent steroid creams must be used under medical supervision. Improper use can thin the skin and cause severe rebound flare-ups.
9. Recognize urgent warning signs
If you experience rapidly spreading redness, severe pain, fever, or extensive scaling, seek immediate medical attention to prevent complications.
Why Choose Dermacian – Your Skin Specialist for Psoriasis in Jaipur
- Experienced dermatologists: Board-certified clinicians who manage the full spectrum—from mild plaque psoriasis to complex psoriatic arthritis cases.
- Technology-forward care: Access to NB-UVB phototherapy and targeted light devices alongside the latest topical, oral, and biologic therapies.
- Personalised plans: We align treatment with your routines, travel, and budget—so it’s practical and sustainable.
- Clear communication: You’ll know the why behind each step, expected timelines, and how to handle minor flares at home.
- Safety & monitoring: Evidence-based protocols, screening before advanced therapies, and scheduled reviews.
- Comfortable, respectful experience: Private treatment areas, patient education, and a friendly team that truly listens.
Looking for a skin specialist for psoriasis who offers both advanced options and empathetic guidance? Dermacian is here to help.
Read More: Top 09 Skin Specialists in Jaipur (2025 List)
Conclusion
Psoriasis is long-term, but suffering doesn’t have to be. With the right diagnosis, a step-wise plan, and consistent follow-ups, most people achieve smooth, comfortable skin and fewer relapses. At Dermacian – Skin & Hair Clinic, Jaipur, we combine dermatologist expertise with modern therapies—from topicals and phototherapy to biologics—to tailor a plan that fits your life.
Ready to take control of psoriasis? Book a consultation at Dermacian today and start your personalised psoriasis treatment in Jaipur. Your clearer-skin journey can begin now.
FAQs
1. Is psoriasis curable?
Not yet. Psoriasis is a chronic condition, but it’s highly controllable with modern treatments. Many patients achieve long periods of clear or almost clear skin with a maintenance plan.
2. How do I know if I need phototherapy or tablets?
If topicals aren’t enough, or large body areas are involved, your dermatologist may suggest NB-UVB phototherapy or systemic medicines. The choice depends on severity, sites involved (scalp, palms/soles, nails), age, pregnancy status, and medical history.
3. Are biologic injections safe?
Biologics are well-studied targeted therapies. We screen for infections and monitor regularly. For suitable candidates, they offer strong, sustained control with structured dosing schedules.
4. How long before I see results?
You can usually start noticing visible improvements in pigmentation within 3 to 6 weeks, though full results may take a few sessions depending on the treatment type and your skin condition
5. What is the cost of psoriasis treatment in Jaipur?
Costs vary by severity and therapy—topicals and light therapy are usually more affordable; biologics are premium options. At Dermacian, you’ll receive a transparent estimate after your evaluation.
6. Can diet or home remedies cure psoriasis?
No diet cures psoriasis, but balanced, anti-inflammatory eating, weight control, and stress reduction can meaningfully reduce flares and improve outcomes alongside medical treatment.